Dr. Anika Clarke, pediatric attending physician, learned of a parent whose lawyer informed her that she couldn’t visit a food pantry because of her immigrant status. But Dr. Clarke and her residents knew otherwise.
“Two months ago, we would have said, ‘If your lawyer said you can’t do that, you probably can’t,’” said Dr. Clarke. “Now we question it, and in this case we referred her to an SBH social worker and gave her a card that contained a list of nearby food pantries that could help her.”
This new understanding stems from the work of Bronx Partners for Healthy Communities (BPHC), SBH’s DSRIP Performing Provider System.
One of DSRIP’s goals is to keep patients healthy by bridging the gap between their medical conditions and their social needs such as food insecurity, housing instability and poverty — all of which impact their health and wellness.
This is particularly relevant in the Bronx where more than 30% of households in some neighborhoods served by SBH live in poverty (data released by NYC Department of Health and Mental Health). The Bronx accounts for more than one-third of legal evictions in the five boroughs (NYC Public Advocate’s Office), and it is estimated that one in four residents live in food-insecure homes (Hunger Free America, 2016).
BPHC, through its partnership with more than 200 Bronx organizations, has been helping SBH residents to better understand the social issues facing patients and the types of community-based services that can support their needs.
“Too often community members are not aware of resources available to them or are reluctant to seek assistance because of misinformation about eligibility or the stigma associated with issues like homelessness, hunger, and poverty,” said Dr. J. Robin Moon, BPHC Director of System Integration.”
Last year BPHC introduced Housing Coordinators from BronxWorks, a Bronx community-based organization, to the Emergency Department to connect patients who are homeless to transitional and permanent housing. Residents have been trained on how to identify patients who may be in need of housing and how to connect them to a Housing Coordinator for further assessment. They also have information on hand for patients about shelters and drop-in centers that can help.
“One result of our work with BPHC is that our doctors know that we have to the ability to address more than just the chief complaint that brought our patients to the ED,” said Dr. Jeffrey Lazar, Medical Director, Department of Emergency Medicine. “We are learning to look at our patients more holistically and consider the underlying issues and social determinants of health that might leave them at risk of not getting better, and potentially needing to return to the hospital if those issues aren’t addressed.”
SBH residents recently participated in a Poverty Simulation hosted by BPHC that provided a powerful look at how poverty and health go hand in hand. Participants had the opportunity to experience the ongoing challenges that many community members who live in poverty face in their daily activities such as buying food and accessing social services.
BPHC also developed BronxResourceDirectory.org, an online, searchable directory of health and social service organizations in the Bronx. Care coordinators, patient navigators and social workers can use the tool to help patients find behavioral health and long-term care providers, housing assistance, food resources, immigration services, and more. (BronxResourceDirectory.org is also available on SBH’s Workplace platform.)
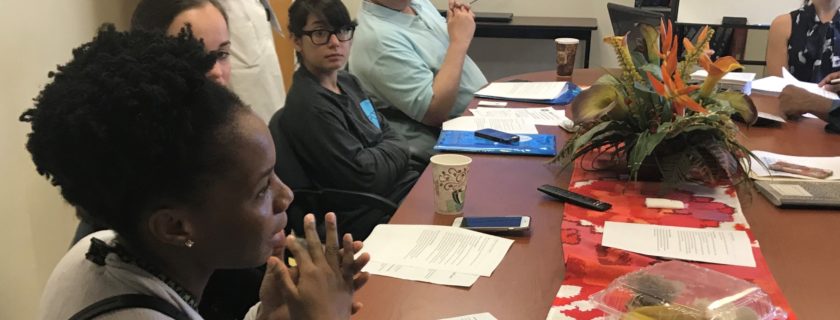
In October, BPHC began a pilot with the Pediatrics Department to address food insecurity among patients and families. BPHC introduced residents to local organizations that provide food and nutrition-related programs, provided guidance on working with care teams, and created patient information with local food programs and other resources.
Analysis of the pilot will be available in a few months but the impact is already being felt.
“I definitely saw that light bulb go off for physicians,” said Dr. Clarke. “They realize that if a patient screens positive for an issue like food insecurity, there is help available. They don’t need to re-invent the wheel; the programs are out there.”
# # #
(printed in SBH Physician Magazine)